Background: Sickle cell disease (SCD) can result in complications affecting multiple organ systems, including renal, pulmonary, and central nervous system. Alkaline phosphatases (ALP) comprise a group of isoenzymes which function to catalyze the hydrolysis of inorganic phosphate monoesters, including phosphoethanolamine, inorganic pyrophosphate, and pyridoxal-5′-phosphate. Predominantly, serum ALP is derived from the liver and bone (1). An elevation in serum ALP primarily signifies hepatobiliary disorders, wherein cholestasis and bile duct damage results in increased enzyme synthesis as a compensatory mechanism. Increased ALP levels can also be an indication of bone disease associated with increased osteoblast activity (2). ALP has been linked to the severity of the pain crisis in SCD (3), and there is also evidence that ALP is a predictor for increased mortality risk in SCD (4-6). This study aims to investigate ALP as a biomarker of SCD severity and acute organ complications (VOE).
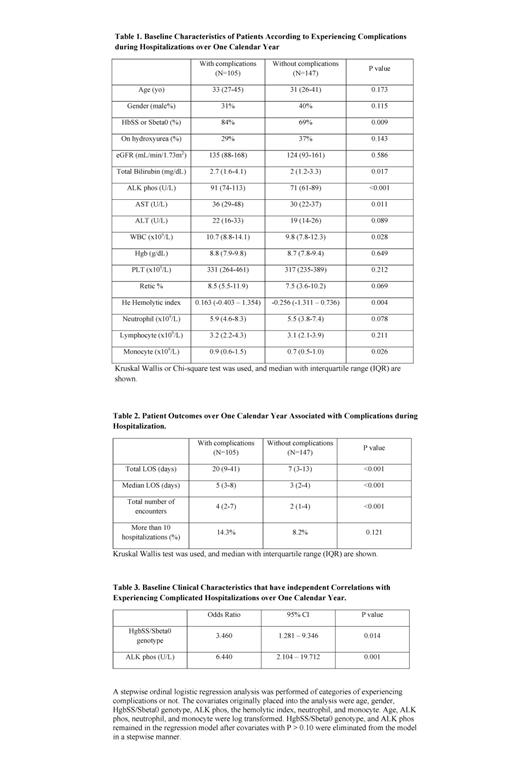
Methods: This retrospective study included 252 patients aged 18 years or older with SCD who were admitted to the University of Illinois Chicago (UIC) hospital for the management of vasoocclusive pain events (VOEs) between July 1, 2017, and June 30, 2018. The study recorded the following complications during hospitalization: acute chest syndrome, acute kidney injury, acute liver injury, thrombotic or hemorrhagic stroke, deep vein thrombosis or thromboembolism, the need for transfer to the intensive care unit, the need for exchange blood transfusion, or death during hospitalization. Data analyses were performed using the Kruskal-Wallis test, Chi-square test, linear or a stepwise ordinal logistic regression analysis.
Results: The median age of this cohort was 31 years (interquartile range 26-42 years), 36% were males and 72% had hemoglobin SS/Sβ0 with 33% on hydroxyurea. In this cohort, 105 patients experienced at least one complication during at least one hospitalization(s) within the one-year study period, while 147 were hospitalized but did not experience complications during the hospitalization (Table 1). A comparison of clinical characteristics between the two cohorts revealed that patients with complications had a higher prevalence of HgbSS/Sβ0-genotype; had higher ALP, total bilirubin, and AST concentrations; Patients with complications had a greater number of hospitalizations and longer length of stay in both the median length and the total length over the study period (Table 2). In a multivariable model comparing baseline characteristics, HgbSS/Sβ0-genotype and increased ALP levels at baseline were significant predictors of complications during hospitalization, after adjusting for other variables as listed in the table (Table 3). Furthermore, in a subgroup analysis of patients with HgbSS/Sβ0-genotype, this relationship was even stronger: higher baseline ALP levels were significantly associated with acute complications during the study period (OR 7.3, 95% CI: 2.2 - 24.1, p = 0.001).
Summary: Our findings suggest that SCD patients with longer hospital stay and higher numbers of admissions tend to have acute complications during hospitalization. Individuals with the HgbSS/Sbeta0 genotype and higher levels of ALP are at an increased risk of developing acute complications, which could potentially account for the increased mortality risk associated with alkaline phosphatase reported by previous literature.
K. Makris, C. Mousa, E. Cavalier, Alkaline Phosphatases: Biochemistry, Functions, and Measurement. Calcif Tissue Int112, 233-242 (2023).
J. Masrour Roudsari, S. Mahjoub, Quantification and comparison of bone-specific alkaline phosphatase with two methods in normal and paget's specimens. Caspian J Intern Med3, 478-483 (2012).
J. I. Brody, W. N. Ryan, M. A. Haidar, Serum alkaline phosphatase isoenzymes in sickle cell anemia. JAMA232, 738-741 (1975).
J. J. Feld et al., Liver injury is associated with mortality in sickle cell disease. Aliment Pharmacol Ther42, 912-921 (2015).
S. A. Curtis, N. Danda, Z. Etzion, H. W. Cohen, H. H. Billett, Longitudinal Analysis of Patient Specific Predictors for Mortality in Sickle Cell Disease. PLoS One11, e0164743 (2016).
V. Sachdev et al., A phenotypic risk score for predicting mortality in sickle cell disease. Br J Haematol192, 932-941 (2021).
Disclosures
Saraf:BEAM Therapeutics: Consultancy, Other: Advisory board; Forma Therapeutics: Consultancy, Other: Advisory board, Research Funding; Novartis: Consultancy, Other: Advisory board, Research Funding; Agios: Consultancy, Other: Advisory board; GBT/Pfizer: Consultancy, Other: Advisory board, Research Funding, Speakers Bureau. Gordeuk:Novartis: Research Funding; Modus Therapeutics: Consultancy; Emmaus: Consultancy, Research Funding; CSL-Behring: Consultancy; Forma: Consultancy, Research Funding; Incyte: Research Funding; GBT/Pfizer: Consultancy, Research Funding; Takeda: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal